The decision to vaccinate is much like a math equation. Someone needs to be confident in the vaccine, want the vaccine, and get a strong provider recommendation. These three things added together almost always mean someone will choose to vaccinate.
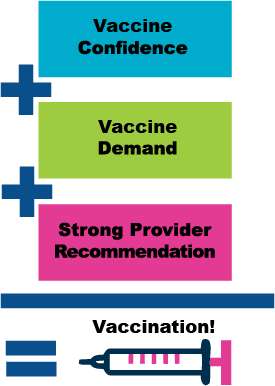
Vaccine Confidence is about understanding the science, the vaccine development process Integrity and vaccine safety. Vaccine Demand is about disease risk perception, vaccine risks and benefits, and removing barriers. A Strong Provider Recommendation is about being a vaccine advocate at every patient encounter.
Increasing vaccine confidence
Vaccine confidence is largely about believing in that vaccines were developed with honesty and care and that they are safe. How can your practice increase vaccine confidence?
Be able to speak to the vaccine development process:
- Make sure your staff understands the rigor of the vaccine development process.
- Hang the vaccine development infographic in your waiting area and exam rooms.
Be knowledgeable about vaccine safety:
- The biggest safety issues tend to be around side effects and ingredients. Be sure you and your staff know the issues.
- Have handouts available to point patients and families to credible information.
Be able to explain vaccine science:
Some healthcare providers don’t think families need to understand vaccine science but research shows this is what families are looking for and what contributes to vaccine confidences so…
- Be sure to be able to easily and understandably explain the science.
- Don’t have the time? Send families to credible websites (shameless plug here – we have an entire science section on our website that was vetted by some of the top vaccine experts in the country.
Make sure your staff are well informed, strong vaccine advocates.
It is self-defeating if a doctor advocates for vaccines, but a med tech or nurse gives conflicting opinions, particularly given they have more time to spend with patients.

Good healthcare workers understand the importance of health science.

All your staff should be pro-vaccine because good healthcare workers understand and support health science. It’s the business they are in after all. The last thing you want is for your staff to be sharing misinformation with patients! If you have staff that don’t support health science, make sure they have the resources they need to be educated on vaccines.
Helpful hints to build a pro-vax staff:
- Provide education to vaccine-hesitant staff – invite them to take the Voices for Vaccines Vaccine Quest!
- Allow time for staff to engage in information and education opportunities for emerging vaccines and VPDs.
- Be clear about your expectation that all staff will be vaccine champions with families and patients
- Include interview questions about vaccine confidence in the hiring process
- Model vaccine positive behavior: Share you and your family’s vaccination status. Have the senior nursing staff do the same.
Well-informed previously vaccine hesitant individuals can be effective vaccine adocates. If you have hesitant staff help them be better informed so they can best advocate for your patients.
Increasing vaccine demand
Vaccine demand is generally about having accurate knowledge of the dangers posed by the disease, understanding the benefits of vaccination, and removing barriers to getting vaccinated.
People do not have good risk perception.
Most vaccines have a one in 1 million risk of a serious adverse event. To put this in context, one-in-one-million is equivalent to:
- ONE single step in a journey of 568 miles
- ONE minute over the course of two years
So one-in-a-million is a very small probability. Families and patients need to better understand the true risks of a disease compared with the small probability of a vaccine adverse event. Having a factual understanding of risks helps caregivers make a truly informed decision about keeping themselves and their families safe.
Understanding adverse events
 Vaccines generally have a risk of 1 in 1 million doses of a serious adverse events. But what does that really mean? An “adverse event” is any health issue that happens after a shot or other vaccine. An adverse event might be truly caused by a vaccine, or it might be pure coincidence. It can be mild like some swelling at the injection site. Or it can be more serious, like trouble breathing. It’s these more serious adverse events that are rare – 1 in one million. And they are usually treatable. So don’t let someone scare you with false information! Vaccines are very safe! Learn more about vaccine safety and vaccine side effects.
Vaccines generally have a risk of 1 in 1 million doses of a serious adverse events. But what does that really mean? An “adverse event” is any health issue that happens after a shot or other vaccine. An adverse event might be truly caused by a vaccine, or it might be pure coincidence. It can be mild like some swelling at the injection site. Or it can be more serious, like trouble breathing. It’s these more serious adverse events that are rare – 1 in one million. And they are usually treatable. So don’t let someone scare you with false information! Vaccines are very safe! Learn more about vaccine safety and vaccine side effects.
People don’t see these Vaccine-Preventable Diseases (VPDs), so they don’t understand how dangerous the diseases are.
Here are some pre-vaccine facts:
What did the world look like before vaccines? It wasn’t pretty. All kidding aside, a LOT of kids died.
Before the measles vaccine, nearly everyone got measles and hundreds died from it every. Today, most providers have not even seen a case of measles because of vaccines!
- Before there was a vaccine for diphtheria, an average of 15,000 Americans would die from it each year. But thanks to
- vaccines, only 2 cases of diphtheria were reported to the CDC between 2004 – 2014.
- In 1964, before the rubella vaccine, an epidemic infected 12.5 million Americans, killing 2,000 babies and causing 11,000 miscarriages. Since 2012, though, there have only been 15 cases of rubella reported to the CDC. Thanks, vaccines!
 We’ve all seen the pins and t-shirts thanking vaccines. Yes, they are pithy and sort of fabulously snarky. But they are also very, very true. We need to help people understand that the only human disease that has been eradicated (wiped from the face of the earth) is smallpox. Every other disease is held at bay by vaccinations. So if we stop vaccinating, the diseases will come back.
We’ve all seen the pins and t-shirts thanking vaccines. Yes, they are pithy and sort of fabulously snarky. But they are also very, very true. We need to help people understand that the only human disease that has been eradicated (wiped from the face of the earth) is smallpox. Every other disease is held at bay by vaccinations. So if we stop vaccinating, the diseases will come back.
What did the world look like before vaccines? It wasn’t pretty. All kidding aside, a LOT of kids died.
Part of vaccine demand is just making it easy to vaccinate.
Use your EHR systems not only to remind caregivers to schedule appointments, but also to prepare them for the vaccines their children will receive and to point them to good information about those vaccines. Ensure all your staff ask about vaccines at every visit.
Giving a strong provider recommendation
Giving a strong provider recommendation Most healthcare providers believe they give strong vaccine recommendations. But studies show that may not always be the case. For instance, during H1N1, only 38% of patients felt they received a strong vaccine recommendation for their children. Thirty-fife percent of patients reported that healthcare providers did not provide any recommendation, and 5% of providers actually discouraged vaccination. We can do better. There are two great models to focus on when providing a strong recommendation. Together, they can instill confidence and drive demand for vaccines. The first model, SHARE, was developed by the Centers for Disease Control and Prevention (CDC). It is a highly effective, evidence-based recommendation model that provides tangible talking points:

SHARE the reasons why the vaccine is right for the patient given his or her age, health status, lifestyle, occupation, or other risk factors.

HIGHLIGHT positive experiences with vaccines (personal or in your practice), as appropriate, to reinforce the benefits and strengthen confidence in vaccination.

ADDRESS questions and any concerns about the vaccine – including side effects, safety, and vaccine effectiveness – in plain and understandable language.

REMIND families that vaccines protect them and their loved ones from serious illness and disease-related complications.

EXPLAIN the potential costs of getting sick, including serious health effects, time lost (such as missing work or school), and financial costs.
Use presumptive positive language.
Research shows that presumptive positive conversations are more effective in positive behaviors than neutral or questioning conversations.
What does presumptive positive look like? It’s stating “it’s time to get your vaccine now” rather than asking “are you planning to get this vaccine.” This works because the majority of us support vaccination and we relate to the way presumptive positive questions make vaccination seem like the normal course of action. Neutral or questioning approaches make us wonder if our choice needs to be examined.
Only delve into the “questioning mode” if someone answers a presumptive positive with “no” or “I don’t know” type answers. Then, find out what their single biggest issue is that is stopping them from getting vaccinated.
- If it’s access: help make it easy to get vaccinated
- If it’s a lack of urgency: help them understand the risks of going unvaccinated
- If it’s information: offer to share understandable and credible information around their biggest concern (shameless plug here, we’ve got TONS of this on our website so send them to us!)

Where did vaccine hesitancy come from?
1998 Lancet paper claimed a connection between autism and vaccines but the study had MAJOR problems:

It made vague conclusions that were not statistically valid

It was not based on medical records but on people’s memory

There was NO control group so it was impossible to determine any association between autism and the MMR vaccine

The conclusions were not based on statistics and the sample size was TINY (12 kids)
Scientists discredited the paper and the Lancet retracted it. But the damage was done. The era of vaccine disinformation was born.
Addressing vaccine hesitancy
When addressing vaccine hesitancy, use the 4-A approach. It helps families feel respected and heard, and empowers them to make positive health decisions.
Four steps. Easy to remember. Winner winner, chicken dinner! Here it is...
“What is your main concern?” Encourage the person to be specific and name what they are most hesitant about. “What is the thing that concerns you most...can you tell me more about it?”
Recognize that the person you are talking to already has knowledge. “It’s clear you’ve really looked into this.”

Affirm that it is OK to have questions. "That's a great question, I heard that too so I looked into it.”
Get permission to share some facts. “Can I share with the facts...” OR “Can I get you some credible sources so your research helps you make an informed decision?”
Learn more about vaccine hesitancy in our vaccine hesitancy toolkit.
© Voices for Vaccines. Excerpts and links may be used by websites and blogs, provided that full and clear credit is given to Voices for Vaccines, with appropriate and specific direction and links to the original content. Parents, providers, advocates, and others may download and duplicate toolkits in print, without alteration, for non-commercial use and with full and proper attribution only.
